SEAS in adults
Over the past 13 years or more, we have published dozens of posts and thousands of comments on our blog dedicated to scoliosis.
The Isico blog is a dedicated space where patients can ask questions and swap experiences, but it is also a place where those involved in treating scoliosis can take a more in-depth look at a series of topics and engage with patients.
SEAS in adults
“You’re too old now”, “Your scoliosis has stopped now that you’ve finished growing”, “If you want to, do some exercise”… How often do adults with vertebral deformities like scoliosis or hyperkyphosis hear things like this?
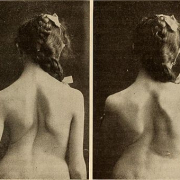
Our patients often tell us that on reaching adulthood they become aware of physical changes, in their back, balance and height, and they therefore start looking for answers and treatments.
The natural ageing process does not spare our back and changes are quite normal and to be expected: when they occur, it is important to get active in order to restore elasticity and strength to joints and muscles. But ageing is an entirely different situation compared with the occurrence of spine deviations in young people, in whom we seek to modify the bone structures and consequently reduce the degrees of curvature.
Scientific studies in recent years have clarified several aspects, that are worth bearing in mind:
1. Scoliosis exceeding 30 degrees at bone maturity, generally reached between 17 and 19 years of age, is at risk of progressing over the years, resulting in a worsening of the existing curves: and the higher the measurement, the greater the risk of worsening.
2. Will scoliosis inevitably lead to back pain? Absolutely NOT!
3. Does having a correct lateral spinal profile (lordosis-kyphosis) protect us against the reduction of our quality of life due to disability and pain? YES, it does.
In light of all this, it is important to know that in adults, too, it is possible to intervene to correct postural abnormalities and prevent and/or slow down the worsening of scoliosis over time: our approach (SEAS) aims to do just this.
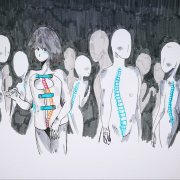
As an effect of the force of gravity, and also the curves that are already present, a scoliotic back will tend to drop down in the direction of the curve, and in many cases, there will also be a forward shift of the trunk. Simple physical activity alone, however useful and beneficial, is insufficient to counteract this phenomenon.
This can only be achieved through specific exercises designed to provide support for the structures of the spine in the opposite direction, and these reinforcement exercises must have precise and individual characteristics, in other words, they must be tailored to the individual patient.
The movements to be carried out must be chosen according to very specific priorities, and this is why it is necessary to turn to qualified professionals who have expertise in dealing with these conditions in adults, using effective approaches.
The SEAS method requires constant collaboration on the part of the patient and seeks to make him “responsible for himself”.
The exercises are carefully worked out for each patient. They are initially performed under the therapist’s guidance and then performed independently, with the patient doing daily repetitions, at home.
Sessions with the therapist are initially scheduled monthly, although this frequency is subsequently reduced, possibly even to only once every three months, and patients are given exercise sheets to follow at home.
It takes at least six months to obtain appreciable results, sufficient to motivate patients to continue and thereby ensure they remain fit well into old age.