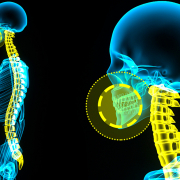
Scoliosis and height: how much does spinal curvature affect stature?
One of the most frequently asked questions regarding scoliosis concerns loss of height:
“My daughter has a 40° scoliosis… does that mean she is shorter than she would otherwise be?”
The answer is not straightforward. Reduction in stature associated with scoliosis does not depend solely on the angle of the curve; it is influenced by a range of structural and morphological characteristics of the spine.
The Cobb angle—commonly referred to as the curve angle—is the standard measure used to quantify the degree of lateral deviation in scoliosis. Over the years, several computational models have been proposed to estimate height loss attributable to scoliosis. However, formulae relying exclusively on the Cobb angle—such as the historical Stokes equation—have proved to be imprecise.
A study by Gardner et al. (2016) demonstrated that the original formula contained an error and emphasised that scoliosis is a three-dimensional deformity that cannot be summarised by a single parameter to estimate height loss. Similarly, Lonner et al. (2016) reported that the Cobb angle alone is insufficient to predict accurately the loss of stature: the true length of the deformed vertebral arc, the number of vertebrae involved and the degree of vertebral rotation all contribute. In other words, two patients with identical Cobb angles may nonetheless exhibit markedly different statures.
Stature is also relevant from a functional and respiratory perspective. Two recent studies from K Politarczyk et al. (2021) have shown that, in individuals with severe scoliosis, measured height may not reflect true body length, thereby affecting the interpretation of pulmonary function tests. In particular, height influences assessment of parameters such as forced vital capacity (FVC)—the total volume of air forcefully and completely exhaled after a full inspiration—and forced expiratory volume in one second (FEV₁). Consequently, in patients with severe scoliosis, it is necessary to correct the recorded height to avoid underestimating actual respiratory capacity.
In summary:
- height loss in scoliosis is non-linear and cannot be estimated solely from the Cobb angle;
- simple formulae, such as the Stokes equation, are now regarded as approximate;
- a more accurate appraisal should incorporate morphological parameters of the curve and trunk, in addition to the Cobb angle;
- for respiratory function testing, consideration of a corrected stature is particularly important in severe cases.
These studies underline that scoliosis is a complex three-dimensional deformity that affects not only appearance and stature but also clinical and functional outcomes. For this reason, assessment and treatment must be individualised and based on a thorough analysis of the curve and the patient’s growth.
Bibliographic references:
- K Politarczyk et al., Stud Health Technol Inform, 2021., Loss of body height due to severe thoracic curvature does impact pulmonary testing results in adolescents with idiopathic scoliosis
- K Politarczyk. et al., J Clin Med, 2021, Differences in spine growth potential for Sanders maturation stages 7A and 7B have implications for treatment of idiopathic scoliosis
- Lonner et al., Spine Deformity, 2016 Measuring anterior trunk deformity in scoliosis: development of asymmetry parameters using surface topography (a pilot study)
- Gardner et al., Scoliosis and Spinal Disorders, 2016, The use of growth standards and corrective formulae to calculate the height loss caused by idiopathic scoliosis