Artificial intelligence and rehabilitation medicine: the revolution has begun
Artificial intelligence (AI) is already a concrete reality at ISICO, where it is actively used in daily clinical practice, as a research tool in studies published in scientific journals, and as part of the European PREPARE project, in which our institute is a partner. AI is fundamentally transforming the work of rehabilitation professionals, opening up new possibilities in early diagnosis, patient monitoring, treatment personalisation, and therapeutic education.
The potential of AI is immense. In a context where the volume of clinical, instrumental and functional data is growing exponentially, intelligent algorithms enable the rapid and efficient analysis of this information, turning it into tangible support for clinical decision-making.
“We are only at the beginning of a transformation that will become increasingly far-reaching” – explains Francesco Negrini, physiatrist at ISICO and Associate Professor at the University of Insubria – “Just as the first computers revolutionised our work in the 1980s, AI is set to become an indispensable tool in the daily work of clinicians”.
In recent years, research on AI in the medical field has experienced a dramatic acceleration. Between 2022 and 2023 alone, funding in this sector increased eightfold, reaching $25 billion. Applications range from imaging diagnostics and outcome prediction to motor rehabilitation support and functional assessment.
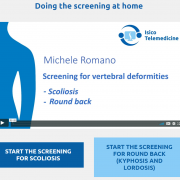
ISICO has contributed to this evolution. One example is a 2023 study on the use of AI to improve scoliosis screening. The team developed an algorithm capable of combining multiple variables (ATR, age, sex, BMI, family history, prominence height, curve location) to detect the condition early — going beyond the limitations of traditional tools like the scoliometer.
But AI’s applications in rehabilitation go far beyond scoliosis. Through data collection from wearable sensors, surface electromyography, and robotic devices, it is now possible to analyse patients’ movements in real time, support the monitoring of gait and speech disorders, classify levels of motor dysfunction, and adapt treatment plans in a truly personalised way.
At ISICO, AI is also used to enhance the patient experience through projects such as ISAIA (ISICO AI Assistant) — a virtual assistant designed to improve communication between clinicians and patients, answer frequently asked questions, and support the management of emails and FAQs. This approach helps maintain an informative and educational dialogue beyond the consultation, responding to patients’ ongoing concerns during treatment.
Another promising frontier is the integration of AI into telerehabilitation. Smartwatches and dedicated apps now make it possible to monitor home exercises with precision, optimising therapeutic pathways remotely. One recent study, for instance, demonstrated that AI could automatically recognise post-stroke rehabilitation exercises with over 99% accuracy.
Of course, with opportunity comes challenge. The handling of sensitive data, the lack of transparency in algorithms (often still “black boxes”), the risk of over-reliance on automated solutions, and the quality of training data are all critical issues requiring careful oversight and regulation. A responsible adoption of AI must be grounded in strong clinical supervision, ongoing human oversight, and the scientific quality of the sources used.
In conclusion, artificial intelligence will not replace clinicians — it will support them, helping them become more accurate, more efficient, and better equipped to offer truly personalised care.
At ISICO, that revolution has already begun.