Scoliosis: is aesthetics measurable?
When it comes to scoliosis therapy, aesthetics is one of the goals along with a healthy back.
Aesthetic deformity due to scoliosis and its impact on the patient is considered by the members of SOSORT (International Society On Scoliosis Orthopaedic and Rehabilitation Treatment) as the most important reason for treating AIS; unfortunately, only a few of scoliosis studies were found in PubMed on this topic.
But can a goal, apparently so subjective, be measurable in a repeatable way to become objective? Yes,according to the data collected by the study Reliability, repeatability and comparison to normal of a set of new stereophotogrammetric parameters to detect trunk asymmetries, recently published by the Journal of BIOLOGICAL REGULATORS & Homeostatic Agents.
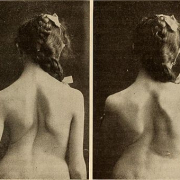
“Aesthetic impairment is a crucial issue in Adolescent Idiopathic Scoliosis (AIS), but to date no objective measurements are available – states Dr Francesco Negrini, Isico physiatrist – for our research, we used the Formetric®, which we usually use to measure sagittal planes. We have established parameters for evaluating symmetries in patients, such as those of the shoulder blades or hips, to obtain objective data related to the aesthetic aspect. In order to validate this instrument for clinical practice, the first step and aim of this study are to evaluate the repeatability of the parameters measured by surface topography in a group of AIS subjects and to test if they can distinguish healthy subjects from AIS patients to develop an objective tool for deformity evaluation of the trunk in AIS patients. For our evaluations, we used a device for surface topography based on the principles of rasterstereography. This device (Formetric®, Diers Biomedical Solutions) can reconstruct digitally in three dimensions the back of any person”.
The study evaluated 15 selected parameters that could be good predictors of scoliosis’ impact on the patients’ trunk.
“We analysed short-term (30 seconds, 38 subjects) and medium-term (90 minutes, 14 subjects) repeatability of surface topography measures and their diagnostic validity in AIS (74 subjects, 33 AIS patients and 41 healthy subjects) – proceeds Dr Negrini – All examined parameters were highly correlated as far as short, and medium-term repeatability is concerned”.
When it comes to aesthetics we cannot stop at Cobb degrees alone, believing that there is no objective measure: “Symmetries can be measured repetitively, as we did in our study – concludes Dr Negrini – so we can offer an objective measurement of aesthetics in patients with idiopathic scoliosis. The surface topography showed good repeatability. Moreover, some of its parameters are correlated with scoliosis, showing that it could very well evaluate deformity due to this pathology. Thanks to these findings, it will be possible to develop a tool that can objectively evaluate aesthetics in AIS patients.”.