Returning to sport after scoliosis surgery: when and why physical activity is part of the treatment
For an adolescent, the prospect of undergoing spinal surgery inevitably raises a fundamental question: “Will I be able to go back to the sport I love?”
In the past, an extremely cautious approach often prevailed. Today, however, scientific evidence clearly shows that returning to physical activity is not only possible but an integral part of the recovery process.
The importance of staying active
Remaining physically active during adolescence is one of the best investments in long-term health. Young patients who stop practicing sport after surgery have a higher risk of developing chronic pain and functional limitations in adulthood.
Unfortunately, studies show that around 30–40% of patients do not return to their previous level of sporting activity. In most cases, this is not due to real physical limitations, but rather to fear (on the part of the patient or parents) or overly strict restrictions imposed by healthcare professionals.
One of the main challenges today for specialists dealing with spinal disorders is to break this vicious circle: a surgically treated body is a body that can — and should — move again.
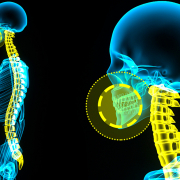
A few words on surgical techniques
Several surgical techniques are currently available. The most commonly used include:
• Spinal fusion (arthrodesis): This is the standard technique. Although it involves immobilising certain segments of the spine, in the vast majority of cases, it allows a full return to most sporting activities.
• Vertebral Body Tethering (VBT): a more recent technique that does not “fuse” the vertebrae but uses a flexible cord. Available data indicate that patients undergoing VBT tend to return to school and sport slightly earlier, although these are often adolescents who were already very physically active before surgery.
The “roadmap” back to sport
Every patient is unique and follows a therapeutic and personal pathway that cannot be identical to that of another patient, even with the same diagnosis. However, the Scoliosis Research Society (SRS) — the oldest scientific society dedicated to this condition — has defined time-based guidelines that reflect the period needed for tissues and instrumentation to stabilise.
In general:
- first 3 months: in most cases, it is possible to resume light sporting activities such as swimming, stationary cycling or gentle jogging, with the aim of rebuilding strength, coordination and confidence in movement.
- around 6 months: many adolescents can return to more demanding dynamic sports such as football and basketball, provided there is no direct contact, gradually increasing intensity and duration.
- 9–12 months: if recovery is smooth and clinical follow-ups confirm good progress, a return to high-impact sports such as rugby, judo and karate is generally allowed.
These indications are not rigid rules, but a reference framework designed to support a safe and gradual return to sport.
Many parents fear that an impact could damage the rods or compromise the nerves. The reality is reassuring: serious complications related to sporting activity are extremely rare.
The most common — though still infrequent — issues involve loosening of a screw or minor damage to the rods, and they tend to occur when recovery stages are rushed (for example, returning to snowboarding after only two weeks).
By respecting healing times and following a gradual progression, the risk remains very low. Surgeons and physiotherapists work together to build a genuine bridge back to normal life, based on trust and collaboration.
The real question is not whether to return to sport, but how and when to do so. Because movement is the medicine that protects the spine over time: returning to sport is not a risk to avoid, but the ultimate goal of every surgical intervention.