Returning to physical activity after surgery for adolescent idiopathic scoliosis
Sport and physical activity are essential for psychosocial and physical well-being in children and adolescents, and youngsters with scoliosis are not subject to any limitations in this regard: they can do sports and other physical activities just like their peers can.
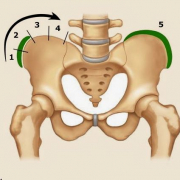
In severe scoliosis, i.e., in individuals with curves measuring more than 50° and presenting significant aesthetic and developmental deformities despite undergoing orthotic/bracing treatment properly administered according to the SOSORT criteria, surgery is indicated.
“In some cases, patients who undergo corrective surgery for scoliosis may reduce their level of physical activity postoperatively due to a loss of spinal flexibility and pain. This inevitably impacts negatively on their quality of life – says dr Carmelo Pulici, physiatrist – No guidelines have yet been published on the resumption of physical activity after surgery for adolescent idiopathic scoliosis, and “expert opinion” is therefore all we have to rely on. Consequently, different surgeons may give different indications, depending on their experience and the particular type of approach”.
There are also individual factors at play, and the decision to resume physical activity may therefore depend on: the type of surgery performed, how the body responds and adapts to the metal rods inserted to correct the spine, the extent of the fusion, how recently the surgery was carried out, the characteristics of the patient, and also the type of sport practised (non-contact, contact or collision).
For example, while some surgeons allow contact sports to be resumed six months after surgery, others recommend waiting a year, and some even rule out the resumption of collision sports altogether (https://pubmed.ncbi.nlm.nih.gov/26920125/).
“In one study, return to sport/physical activities after surgery was examined using a specially created questionnaire (https://pubmed.ncbi.nlm.nih.gov/28604495/). By six months, most patients had returned to the activities they did before the surgery” – explains Dr Pulici. “The authors found that patients returned to athletics much earlier than expected. Despite this, there were no cases of loss of correction, implant failure or complications among the 95 patients included in the study”.
A new surgical technique
In recent years, there has been a growing interest in vertebral body tethering (VBT), a new surgical technique used only in children and in early adolescence and, even then, only in carefully selected patients, given that the method is still experimental. VBT is proposed as a possible alternative to spinal fusion (currently the most widely used technique for the surgical treatment of scoliosis). Unlike spinal fusion, it does not reduce the mobility of the spine.
“According to a recent study, VBT allows daily activities and sports to be resumed within three months of the surgery” Dr Pulici goes on. “Furthermore, most of the patients examined in the study reported an improvement in their athletic performance, and some were found to be doing more sports than before undergoing VBT”.
Even though surgeons today tend to allow patients to return to sports (even high-intensity ones) earlier than in the past (https://pubmed.ncbi.nlm.nih.gov/34267153/), we are still a long way from seeing a common approach to the management of postoperative resumption of physical activity in this patient population.
In the absence of guidelines, we at Isico recommend that patients turn to an experienced therapist in the post-operative period to ensure a gradual and safe return to physical activity, obviously following the instructions received from their surgeon.
It is important to avoid falling into the vicious cycle of a sedentary lifestyle. The less active you are, the less you feel inclined to do physical activity and the greater the risks to your health due to your lack of movement.