Daytime versus night-time bracing: what to do when scientific evidence is of no help?
When we sit down in front of a doctor, we often expect him or her to have the solution to all our problems, but of course this is not the case. Unfortunately, that isn’t how evidence-based medicine (EBM) works!
EBM is defined as the explicit, conscientious and judicious use of the best current scientific evidence in decision making regarding the treatment of an individual patient or population. Indeed, the term “evidence” refers not to that which is “evident”, but rather to what has been discovered through specific research.
Evidence-based clinical practice is built on 3 key elements:
– the best research evidence;
– the clinical experience of the treating physician;
– the patient’s values and expectations.
In other words, optimal clinical decision-making is based on knowledge of the best available scientific evidence, which must be combined with the values and preferences of the patient, who is involved directly in the process of choosing his or her treatment.
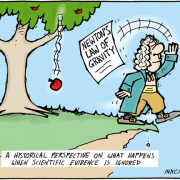
But scientific evidence cannot answer all the questions that crop up in medicine. In the field of scoliosis treatment, for example, there are no studies showing that brace wearing is more effective during the day than at night.
So, what are doctors meant to do when they are faced with situations like this? In the absence of available scientific evidence, the decision has to be based on the other two foundation stones of clinical practice (the doctor’s personal experience and the patient’s values), so as to achieve the best possible outcome.
As far as bracing is concerned, there is an important study “Adolescent Idiopathic Scoliosis Bracing Success Is Influenced by Time in Brace: Comparative Effectiveness Analysis of BrAIST and ISICO Cohorts” which shows that the outcome, in terms of curve correction, depends on the number of hours the brace is worn: the longer it is worn the better the result will be.
On the basis of this knowledge, and also with the aim of increasing our patients’ compliance with the treatment, we at ISICO have decided that patients should always wear their brace at night, and enjoy their brace-off hours (as prescribed by their doctor) during the daytime.
After all, if patients sleep without their brace on, this means they lose 7-8 hours of correction every 24 hours. What is more, using brace-off hours during the daytime makes it easier for youngsters to take part in the daily activities they enjoy (sports, going out with friends, and so on), and this increases not only the level of compliance with the treatment, but also their quality of life.
Finally, we know that our spine does not remain passive during sleep; on the contrary, when we are in bed, swelling of the intervertebral discs (shock-absorbing “sponges” situated between our vertebrae) causes lengthening and tension of this entire structure, which is so important in growth.
This is one of the reasons why ISICO (and pretty much all practitioners worldwide) now recommend that, when the time comes to do so, bracing hours should be reduced during the daytime, until the point is finally reached when patients, in the last months of their treatment, are wearing their brace only at night. This, then, is an example of how the clinical experience of a specialist team and the particular needs of patients can together serve as the basis for making sound therapeutic choices in the absence of hard scientific evidence.