What is secondary scoliosis?
Scoliosis: idiopathic or secondary? Let’s look at the difference.
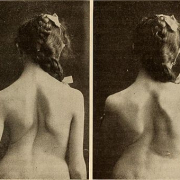
Scoliosis, defined as a “three-dimensional deformity of the spine”, affects 3% of the population overall, and in 80% of cases its origin is not known. In these cases, it is therefore termed idiopathic.
In the other 20% of cases, on the other hand, the cause of the scoliosis is known; in these cases, it is secondary to another condition.
In particular, scoliosis can be the manifestation of congenital defects, i.e. abnormalities that originate before birth, such as abnormalities of vertebral formation like rib or vertebra fusions. It can also occur in inherited genetic syndromes, involving the nervous and/or musculoskeletal systems, and in diseases such as neurofibromatosis, Marfan’s disease, Willi-Prader syndrome and syringomyelia.
In a further subgroup of cases, scoliosis can be secondary to iatrogenic causes, i.e. a “side effect” of medical treatments such as radiotherapy, or surgical procedures such as laminectomy or thoracotomy.
Finally, scoliosis can also have other causes, such as burns or retracted scars, post-traumatic paraplegia, spinal tumours, or bacterial or parasitic spinal infections.
The specific features of secondary scoliosis, including the mean age at onset, closely depend on the disease with which it is associated. Overall, these forms are more aggressive and less treatment responsive than idiopathic scoliosis.
In all these cases, whether secondary scoliosis is suspected or has already been diagnosed, it is crucial to consult a medical spine specialist.
If the cause of the scoliosis is not clear the specialist, after performing an in-depth clinical and instrumental evaluation, will refer the patient for further investigations and tests, necessary to confirm or exclude the presence of primary conditions “masked” by the scoliosis.
Once secondary scoliosis is confirmed, the proposed treatment and its management over time will be planned and adjusted taking into account the patient’s overall condition and its complexities.
Precisely because these forms are often particularly aggressive, it is crucial to contact extremely competent specialists in the field of spinal disorders, in order to start monitoring the evolution of the disease. Only in this way can the best therapeutic and rehabilitation options be identified, on the basis of the patient’s overall conditions and the opportunities, benefits and objectives identified.
The spine specialist will thus intervene with the agreement of, and in collaboration with, the various healthcare professionals involved in the patient’s care. This multidisciplinary approach is necessary to ensure that every aspect of the patient’s condition is considered in the effort to optimise his/her health.